Abstract
Introduction: The neurologic changes of sickle cell anemia (SCA) are particularly devastating and include acute stroke, silent infarctions, and cerebral hypoxemia that together result in cumulative damage and significant neurocognitive deficits. Executive functioning and attention are the most commonly reported deficits with individuals with SCA scoring on average ten points lower on measures of full scale intelligence compared to matched unaffected controls, translating to poor academic achievement and later job attainment. Hydroxyurea is the standard-of-care in patients with SCA with a growing body of evidence suggesting a role in neuroprotection. However, although encouraging, until now, the only studies have involved children who began hydroxyurea in grade school, well after the onset of SCA-related neurocognitive decline. Beginning in 2014, Cincinnati Children's Hospital Medical Center (CCHMC) began treating children with SCA as young as six months with hydroxyurea; these children have had few SCA-related complications and offer a unique population to evaluate the effects of the early introduction of hydroxyurea on neurocognition.
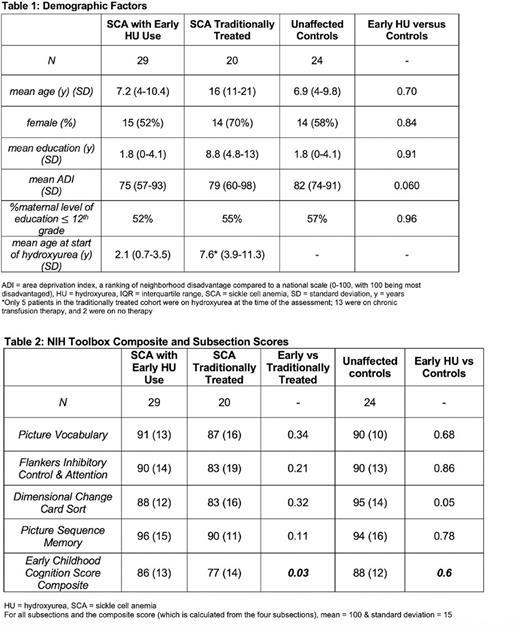
Methods: We completed a cross-sectional analysis of the neurocognitive status of our SCA population. Children at least three years old with SCA were enrolled in two cohorts: 1) children with SCA (HbSS and HbS-B 0thalassemia genotypes) who began hydroxyurea before age five years and 2) children with SCA who did not qualify for the first cohort (either on hydroxyurea or chronic transfusions (CTT)). Unaffected controls (siblings of patients with SCA or children seen in the CCHMC primary care clinic) were matched to each patient with early hydroxyurea use by age, race, and sex. All participants completed the NIH Toolbox: Cognition Battery, a shortened neuropsychological evaluation administered using a handheld tablet in the clinical setting, requiring 15-30 minutes. The mean score is 100 and standard deviation 15. We also obtained academic history, demographic variables, and laboratory values for SCA patients.
Our overall objective was to compare the neurocognitive status of children with SCA who initiated hydroxyurea before age five years to an unaffected, matched sibling and community control cohort and to historically treated patients followed at the CCHMC sickle cell clinic in order to assess whether the beneficial effects of hydroxyurea extend to neuroprotection.
Results: We enrolled 29 patients into the early hydroxyurea SCA group with 24 matched unaffected controls (early hydroxyurea group: mean age 7.2 +/-3.2 years, 52% female). The SCA cohort who initiated disease modifying treatment later in life included 20 patients (mean age 16 +/-5.1 years, 70% female) (Table 1). There were no differences in age, gender, patient education, maternal education, and Area Deprivation Index (ADI, a marker of socioeconomic status) between the early hydroxyurea SCA and control cohorts (Table 1). In the SCA cohort initiating treatment later in life, 5 patients received hydroxyurea, 13 were on CTT for reasons other than for stroke prophylaxis, and 2 received no therapy. The early hydroxyurea use patients and controls scored no differently on the composite cognition score (86 +/-13 versus 88 +/-12, p = 0.6), while the early hydroxyurea patients scored significantly higher than the SCA cohort treated later in life on the composite cognition (versus 77 +/-14, p = 0.03) (Table 2). On a linear regression model, age (p = 0.004) and patient years of education (p = 0.04) were significantly correlated with the composite cognition score when considering all cohorts. When limited to only patients with SCA on hydroxyurea, age (p = 0.005) and patient education (p = 0.002) remained significant, while maternal educational attainment below high school (p = 0.07), hemoglobin (p = 0.07), and fetal hemoglobin (p = 0.07) approached significance.
Conclusions: Due to challenges with social determinants of health, children with SCA are already at risk for poor academic performance with early and recurrent "silent" hypoxic events further exacerbating these challenges. If started early in life and maintained through the important early years of brain development, hydroxyurea may be neuroprotective for children with SCA. These data provide further evidence to support the universal prescription of hydroxyurea beginning in the first years of life for all children with SCA.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal